Anatomy and Function of the Prostate
Prostate gland is situated below the bladder in males and surrounds the urethra. The weight of the prostate gland is about 25-30g in adult males. The main function of prostate is to produce the liquid part of the semen and helps ejaculation of this fluid during the sexual intercourse.
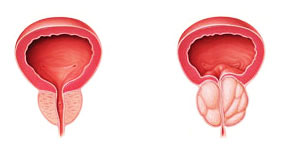
Beginning from the age of 40s, prostate gland starts to enlarge. Particularly the inner portion of the prostate may enlargen and as a result, prostate gland which has a normal size of a chestnut, becomes as large as an apple and even an orange. Medically, this is defined as benign prostatic hyperplasia and people call it prostate enlargement. Studies show that 50% of men at 60 age and 90% of mean at 80 age display benign prostatic hyperplasia. BPH and prostate cancer are different conditions. While BPH do not lead to prostate cancer, they may coexist.
While enlargening, prostate obstructs urinary tract and starts to prevent urine from flowing to the urethra. During the course of this disease, patients start to state complaints about their urinary functions depending on the level of obstruction. The complaints of the patients are evaluated in 2 main groups:
Obstructive complaints
- Weaker and thinner urinary stream
- Difficulty in initiation of the voiding
- Intermittent urination
- Post-urination dribble
- Sense of incomplete bladder emptying
- Hematuria
Irritative complaints
- Frequent urination
- Sudden need to urinate
- Incontinence-involuntary leakage of urine
- Dysuria and pain while urinating
In some instances, urinary tract may exhibit a sudden obstruction due to BPH and inhibit urination which requires immediate catheterization.
The enlargement of prostate in BPH is not a very important sign by itself. The accompanying signs such as occurrence of complaints, increase in degree of complaints, and the negative effects inflicted by the enlargement, all contribute to the importance of the disease.
Negative effects (complications) of BPH on urinary tract are listed below:
- Sudden urinary obstruction: Urinary tract is obstructed completely and prevents patient from urination. Consequently, a severe pain occurs in the lower abdomen. A catheter should be inserted through urethra and the accumulation of urine in the bladder should be emptied.
- Urinary tract inflammation: Inflammation may arise in the urinary tract as a result of the obstruction. In this condition, patients may complain about a severe sense of burning and high temperature.
- Bladder disorders: Due to the obstruction of bladder by prostate, the bladder can not empty its content and as a result enlargens, weakens, and may lose its ability to contract in time. The loss of contraction ability leads to formation of urine residues in the bladder. Sometimes, this problem may not be solved despite surgery.
- Bladder Stones: Bladder stones may form as a result of the inflammation of the accumulated urine or precipitation of the minerals in the bladder.
- Renal disorders: Bladder inflammations may affect kidneys. Moreover, because of the pressure increase as a result of the bladder obstruction and continuous formation of residual urine in the bladder, kidneys may exhibit enlargement and dysfunction in time. Rarely, renal failure may arise in some cases.
Operation is required in patients having those conditions.
Diagnosis of BPH
Sometimes, the underlying cause of the urinary complaints may not be prostate enlargement (e.g: diabetes, diuretics, urinary tract inflammations, bladder cancer, neurological disorders of the bladder, and urethral stenoses). Therefore, in order to diagnose benign prostatic hyperplasia, a thorough history of the patients should be taken. Diabetic patients often display more frequent urination. On the other side, a patient with early period BPH shows increase of complaints if antihistaminic or decongestant is used against cold. Other than those, these patients will probably be asked the following questions:
- What are your complaints?
- How long have you been experiencing these complaints?
- How frequently you suffer those complaints?
- Is it getting worse?
- Do you have anyone in your family who has a history of prostate disease (particularly prostate cancer)?
- Do you use any drugs, if you do, what are they?
Digital Rectal Examination (DRE)
The physician examines the size, consistency, and shape of the prostate by DRE. In benign prostatic hyperplasia, prostate presents with an elastic consistency and elevated volume. Any firmness in the prostate should be suspected as cancer.
PSA Test
Prostate gland produces an enzyme called as Prostate Specific Antigen (PSA) which generates the consistency of the semen. A small portion of this blends into the blood flow. While increase in blood levels can be observed in BPH or prostate inflammation, prostate cancer may increase its level in blood flow, as well. When age-specific PSA values (for example it should be lower than 2 ng/ml in men below 50 age whereas it should be lower than 2.5ng/ml in individuals between 50-60 age) are high and firmness is determined during rectal examination, prostate cancer should be eliminated definitively. As every PSA rise does not mean presence of cancer, there may be a cancer in cases where PSA is normal
Urinalysis
In case there are inflammatory cells or blood cells in the urinalysis, other diseases that could lead to this result should be eliminated (e.g.: urinary tract inflammations, urinary tract calculi, bladder tumors etc.).
Urine Flow Rare
Normal maximal urine flow rate is 15ml/s and average flow rate should be 10ml/s. Normal urination duration is 30 seconds (half a minute). If prostate obstructs the urinary tract in BPH, those values display a decrease and duration of urination elevates. In order for this test to be reliable, the urine amount should at least be 150ml.
Ultrasonographic Analysis
By employing sound waves, one can gain information from abdominal surface or rectal tract on size and inner structure of the prostate along with the changes it inflicted on urethra. Rectal ultrasonography is also used for the procedure of prostate biopsy.
Prostate Symptom Score Calculation
By this method which is called as IPSS, the complaints of the patients can be graded. Following medical or surgical treatment, it may be employed to evaluate the efficiency of the treatment in the follow-up period.
PVR (Postvoidal Residual) Analysis
Determination of the residual urine in the bladder following urination. Generally, it is performed by a special ultrasound device called as “bladder scan”. By insertion of a catheter through urethra, the assessment can be accomplished more precisely however this is a method, which causes discomfort among patients.
Urodynamics, Pressure-Flow Study
When the complaints associated with urination are suspected to originate from prostate enlargement (particularly among young or very old patients; patients who do not exhibit large prostate size), by inserting a catheter through the urinary tract, several parameters such as bladder pressure, urinary tract flow rate and pressure can be measured with a urodynamics device. Thus, it can be determined whether the complaints of the patient originate from bladder contraction disorders or not.
Cystoscopy
This is a method in which a device called cystoscope is inserted through the urinary tract under local anesthesia in order to understand the extent of the urinary obstruction and determine a disease other than prostate enlargement in the urinary tract.
Intravenous Urography or Computed Tomography *
In cases where there is a blood cell in the urine along with prostate enlargement or stone diseases are suspected, it is used to obtain further information on kidneys and urinary system by intravenous delivery of a radio opaque agent containing iodine or thin section tomography images.
* It can not be applied on patients with a creatinine level higher than normal.
Treatment of the Benign Prostatic Disease:
A) Non-Surgical Treatments
Follow-up: Presence of BPH does not mean that it should be treated. In patients who do not exhibit difficulty in urinary flow and associated signs and symptoms where urologic evaluation reveals no damage in kidneys or bladder, the patient may be put under monitorization process. The follow-up period can be 1 year at longest and the visits are planned by the physician.
Medical Treatment: Treatment is started when BPH symptoms start to intervene with the daily activities and quality of life of the patients. Generally, drugs are the first choice of treatment.
5-alphareductase inhibitors: Finasteride (Prosterid, Proscar, Dilaprost) and dutasteride (Avodart) are a few examples. They show their effect by inhibiting testosterone to its active form dihydrotestosterone (DHT). They are reported to decrease the size of prostate by this effect. Libido loss, impotency (loss of sexual function), enlargement and tenderness in the breasts, and reduction in number of sperms are known to be their adverse effects.
Alpha-blockers: By relaxing the smooth muscles localized in the bladder neck and prostate, they cause dilatation of the urinary tract. Taken once a day P.O. Alfuzosin (Xatral), Doxazosin (Cardura), Terazosin (Hytrin), Tamsulosin (Flomax) are the best known of those agents. Adverse effects are headache, dizziness, exhaustion, weakness, and reduction in blood pressure.
B) Minimally Invasive Treatments:
Prostatic stent procedures: It may be applied on cases which can not be operated due to poor overall health status despite requirement of surgery and which do not respond to medical therapies. It is a spiral device that is placed through a thin tube which dilatates urethra when opened. Urolume and Memotherm may be quoted here as the most frequently employed stents. It has some advantages such as needing no general anesthesia or hospital stay, considerably lower risk of hemorrhage, and applicability in shorter time. Possible major disadvantages are misplacement or displacement of the stent, irritation and irritation-related frequent urination, urinary incontinence, and pain.
Transurethral Microwave Treatment (TUMT)
Transurethral Microwave treatment is a method used for reducing the size of the prostate tissue. A microwave antenna attached to a catheter is inserted through the urethra and close to the prostate tissue. The antenna emits a certain amount of microwave energy and increases the temperature of the prostate tissue. While prostate tissue is heated, the surrounding tissues should be protected. The serum flowing around the microwave antenna during the procedure, protects urethra from heating. Moreover, the microwave energy level is elevated gradually during the procedure whereas the heat elevation in rectum and urethra is controlled via sensors in those areas. In case a harmful rise of temperature occurs, the system shuts itself off automatically.
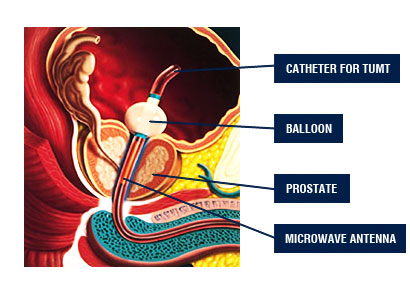
Transurethral microwave procedure is a method which lasts for 30-35 minutes and can be performed with local anesthesia. Sometimes, intravenous sedatives may be required. Patients may feel a rising temperature in urethra or around prostate. Also, as a result of the contraction of the bladder, excessive need for voiding may arise. After the end of the treatment, all those complaints cease. A urinary catheter is left in the patients for 1 week after the procedure. After removal of this catheter, patients may experience frequent need to urinate, sense of incontinence, pain while urinating, and hematuria for 2-3 weeks. Most of the patients return to their normal lives and sexual activities in 1-2 weeks.
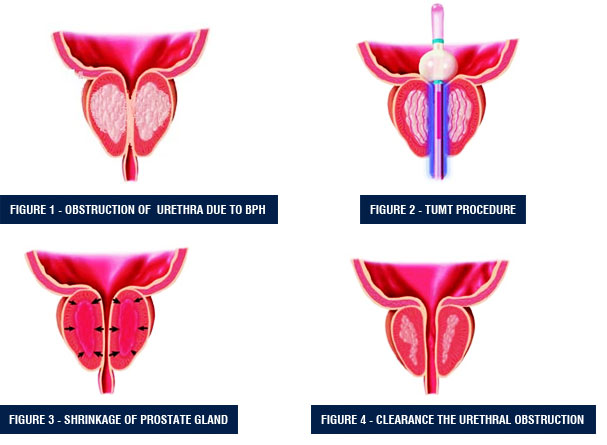
Transurethral microwave treatment benefits patients who has a prostate showing moderate enlargement and experience moderate urinary complaints. It can be applied easily on patients who use blood thinners such as Coumadin and Aspirin. This method may not work in cases where the prostate region called as middle lobe enlargens onto the bladder. This method should not be applied on patients who had experienced radiation on pelvic region or exhibit stenotic urethra. Moreover, it should also not be applied on patients with penile prosthesis or artificial sphincter.
Regarding the results, TUMT is more effective in accelerating the urinary flow compared with the drug therapies. While 40-70% improvement is achieved in urinary complaints of the patients, it also produces a 14-60% improvement in urinary flow rates. Transurethral microwave treatments cause less complications than transurethral prostate resections. Prolonged catheter time, irritative symptoms, and dysuria (sense of burning while voiding) are the most common possible complications.
Currently, transurethral microwave treatment seems to be a reliable alternative for other operation methods due to the obtained good results and no anesthesia requirement.
Transurethral Prostate Resection (TURP)
Transurethral prostate resection is the most commonly applied method in surgical treatment of benign prostatic hyperplasia (BPH). In this method, following general or lumbar (spinal or epidural) anesthesia, a special device called as resectoscope is inserted through the urethra and prostate tissues are resected by employing electrical current. By the help of an optic, the interior view of the patient is transferred to a monitor. The operation is carried out with the guidance of images magnified x10-12 times and irrigation fluid should be used all along this procedure. Electrical current is delivered to the tissues by a crescent-shaped wire called as “loop” and while prostate tissue is sliced into stripes, loop is employed for achieving hemostasis. Prostate tissues accumulated in the bladder are eventually removed with a vacuum system. Following the operation, a urethral catheter is placed and left there for 2 days.

The major advantages of transurethral prostate resection are known to be formation of a cavity by removal of the obstructive portion of the prostate in a short time and the capability to evaluate the removed tissues. Although rarely, a hemorrhage which does not require blood transfusion may occur before or during the operation. Also, postoperative stenosis of urethra may be observed in some cases.
